BY HANS DUVEFELT
I have written many times about how I have made a better diagnosis than the doctor who saw my patient in the emergency room. That doesn’t mean I’m smarter or even that I have a better batting average. I don’t know how often it is the other way around, but I do know that sometimes I’m wrong about what causes my patient’s symptoms.
We all work under certain pressures, from overbooked clinic schedules to overfilled emergency room waiting areas, from “poor historians” (patients who can’t describe their symptoms or their timeline very well) to our own mental fatigue after many hours on the job.
My purpose in writing about these cases is to show how disease, the enemy in clinical practice if you will, can present and evolve in ways that can fool any one of us. We simply can’t evaluate every symptom to its absolute fullest. That would clog “the system” and leave many patients entirely without care. So we formulate the most reasonable diagnosis and treatment plan we can and tell the patient or their caregiver that they will need followup, especially if symptoms change or get worse.
Martha is a group home resident with intellectual disabilities, who once underwent a drastic change in her behavior and self care skills. She even seemed a bit lethargic. A big workup in the emergency room could only demonstrate one abnormality: Her head CT showed a massive sinus infection. She got antibiotics and perked up with a ten day course of antibiotics.
A month later, her condition deteriorated again. It was on the weekend. This time she had a mild cough. Her chest X-ray showed double sided pneumonia. She got antibiotics again and started to feel better.
When I saw her in followup, she was still coughing a little, and she wasn’t her usual happy self. Her lungs were clear. I asked her caregiver if they had done a head CT the last time she was in the ER. I saw no mention of it in the ER report.
“I’m pretty sure they did”, he said.
I retrieved it from the statewide Maine Health InfoNet site. It described that all the sinuses were infected and only slightly improved from the earlier study.
Martha is now on a much longer course of antibiotics, because a sinusitis often takes a lot longer to clear up than most pneumonias. I sometimes compare this to getting the contents of an egg out through a tiny hole in the shell (I never did learn how that is done). And, a sinusitis can sometimes cause pneumonia because of postnasal drip.
I saw another case the other day where I think I was able to piece things together.
Gretchen had seen another provider for headaches. She had migraines in her youth but they stopped after she had her first child. My colleague ordered a brain MRI to make sure there wasn’t something more malignant going on. It showed what the radiologist described as a possible migrainous angiopathy.
By the time I ended up seeing her, she had had the migraine for over a week and she had taken daily doses of over-the-counter remedies, so I figured that she now had an element of withdrawal headache. Normally I prescribe prednisone in such cases, but Gretchen told me she has had severe psychiatric side effects from steroids before.
I asked her to wean off the OTC medications and started her on topiramate. Gradually her headaches got better. Then, a few days later we got a phone call, saying her migraine had come back with a vengeance. It was late in the day and she had been vomiting. She went to the ER and they gave her IV fluids, metoclopramide and something for pain.
I saw her in followup and she was better but very worried, telling me her headache was starting to build again.
Then she told me something that jolted my brain I to action.
“Whenever I start to hurt on the side of my nose where I had the surgery, the headache comes on.”
“What kind of surgery”, I asked.
“I had a big cyst removed, se-ba-cious I think it was called.”
“Can you take your mask off”, I asked. I had not seen her uncovered face before.
She did and there was a big scar.
“What kind of pain do you have there”, I asked. Is it steady or, like, pulsating?”
“It’s like jabs and jabs, like someone is sticking needles in there.”
I pulled the monofilament from my pocket and started touching her over the three branches of the trigeminal nerve on each side of her face.
“Does this feel the same on both sides of your face?”
“No, it’s different.”
I took a deep sigh and explained:
“This looks like a nerve pain, a neuralgia, in the nerve that reaches the skin outside your sinus there, and also in the other two branches that go to the forehead and the jaw. It’s called the trigeminal nerve and it comes directly from the brain. I wonder if that is what has made your migraines come back after all these years.”
“Can you stop this from getting full blown”, she asked.
“I probably can’t stop the neuralgia very quickly. Most neuralgia medications take a while to,start working, but I’ll send in a prescription for Imitrex. Take one as soon as you get home and you can take one more later today if you have to. Then call me tomorrow and let me know how you are doing.”
The next day she told me she was headache free after just one Imitrex, and the neuralgia was barely noticeable.
I’m curious how she will do in the long run, and I’m curious if the trigeminal neuralgia is somehow related to the surgery she had there.
Like I’ve said before, curiosity is a powerful antidote to burnout.
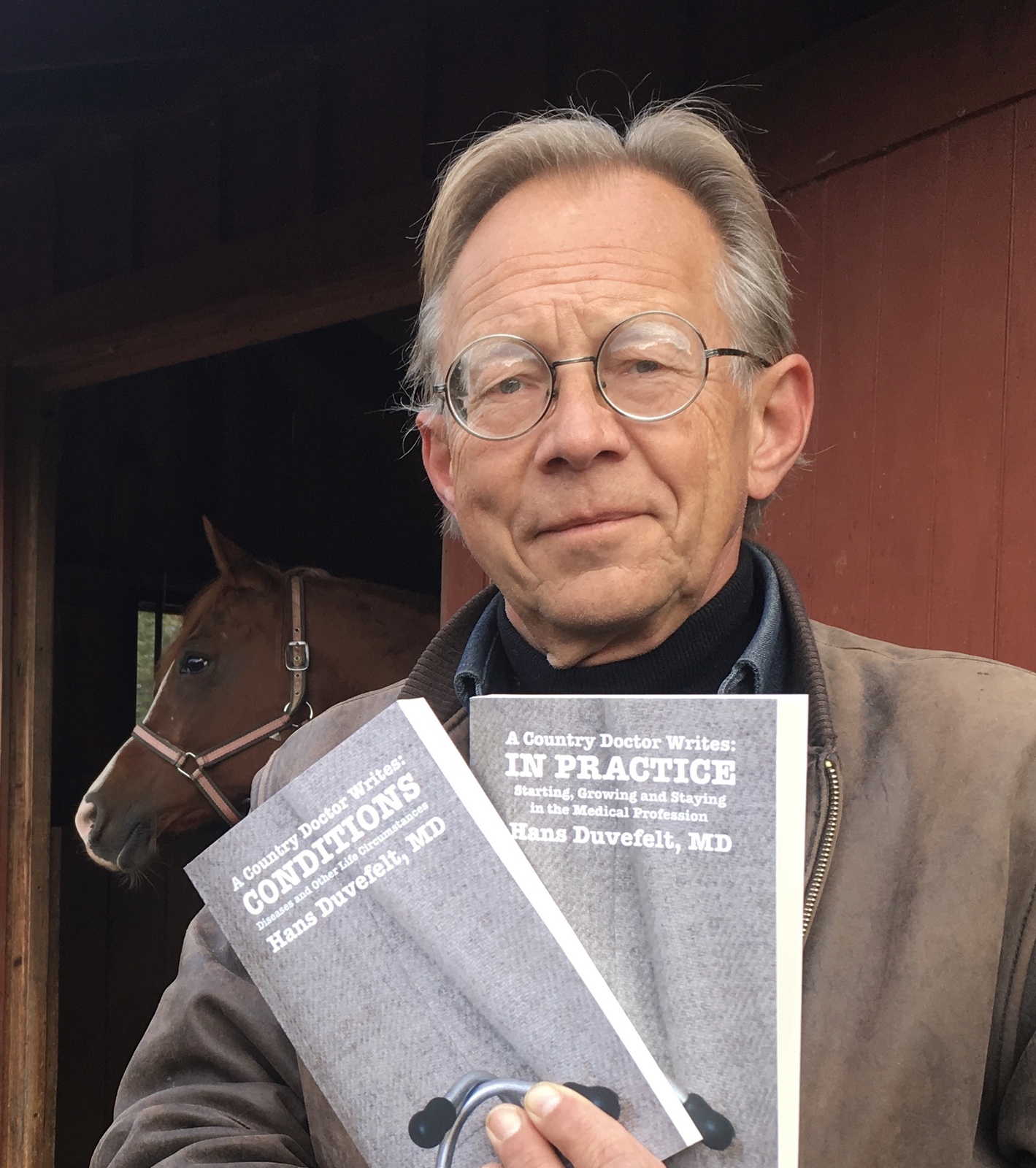
Hans Duvefelt is a clinician, writer, and author of “A Country Doctor Writes.”