Home health aides regularly work “below” the top of their licenses. That’s an inefficiency more and more providers are looking to address.
Sentara Health is a Virginia-based health system with 11 home health locations in both Virginia and North Carolina. Sherry Kesler runs the home health arm as the director of home health services.
In November 2021, Kesler and the rest of her team created a pilot that started with a “top of license” steering committee to get a better sense of how their clinicians wanted to operate.
“We know it is job satisfying to work at the top of license for clinicians,” Kesler said at the National Association for Home Care & Hospice’s (NAHC) annual conference Tuesday. “We know that doing clerical work in a home care visit is not the most satisfying part of a home care visit. At the same time, we knew that overhauling how we deliver in-home care was going to challenge staffing time. But patient access to care is obviously critical, and we had to ensure that whatever we were adding or taking away was a value-add to how we operate.”
The pilot program came from the understanding that “clinicians are not comfortable with virtual care,” Kesler said. That’s where Sentara started.

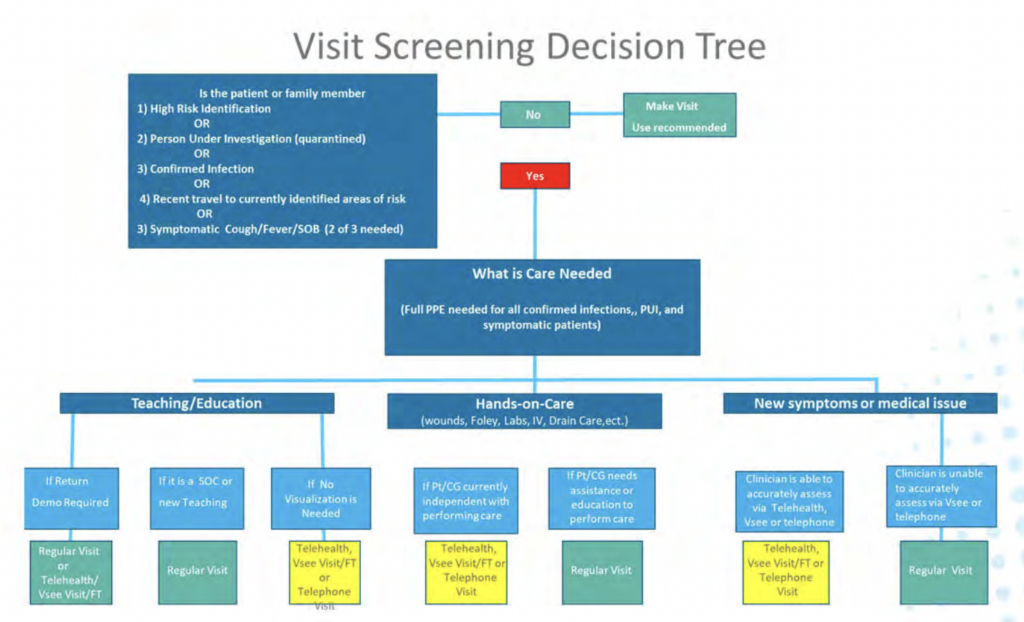
Source: Sentara Health
As part of the care model overhaul, Sentara created the above chart as a way to coordinate what could and could not be done virtually — all with clinician and patient input.
“It was really important for us to have a feedback mechanism,” Kesler said. “We had a daily huddle with clinicians and staff, we did customer service calls with patients to get their feedback and we used our marketing team in the hospitals to make sure there wasn’t any negative feedback.”
The results after six months were impressive.
With the new model in place – and operating in a more efficient workflow structure – the average time to perform a start of care visit dropped from 117 minutes to 88 minutes.
Staff turnover fell from 27% to 16%, 30-day readmission rates fell from 12.8% to 12.6%, and the denial rate fell from 29% to 20%.
Other KPI score standouts included a 14.8% drop in visits per episode, a 9.6% drop in total visits and a 3.25% increase in PDGM visits.

Source: Sentara Health
Meanwhile, the investment required was minimal. Sentara cited only a 0.76% increase in salaries during the first six months of the new program.
Home health providers’ evolution
For Vince Moffit, the CEO of Basin Home Health & Hospice, forward-looking change has been around developing client-driven care models.
“One of the big things we’re doing is focusing on a more client-driven care model,” Moffit told Home Health Care News. “We’ve made an effort to pull more of that information into our offices through care coordination and working with our clinicians to make sure we’re scoring our OASIS efficiently and things like that. If we’re doing it right, not only are we going to see benefits in our reimbursement rates and our STAR ratings, the patient’s going to get better.”
Basin Home Health & Hospice is a New Mexico-based provider with 700 employees. It serves the rural communities in the Four Corners area.
Over the last few years, Moffit and his team have shifted their mindset away from the quantity of in-home visits to a more value-based approach.
Like Sentara, Basin has started to rethink its in-home visits. Through this transition, Moffit has learned that a lot of efficiencies can be found in-between visits.
“A lot of what we’re doing is based on the education we give the patient and the caregiver,” he said. “That way we can ensure that if something happens or there are things going on between our visits after we leave a patient’s home, they have the skills to be able to handle that.”
With reimbursement rates tied to value and patient outcomes, those in-home visits become even more critical — especially early on.
“Another real strong focus of ours has been identifying things during a visit that can lead to rehospitalization,” Moffit said. “Once again, it’s about educating the patient. They don’t want to go back to the hospital, we don’t want them to go back and the hospital doesn’t want them to come back.”
Some indicators include fluctuating weight, blood pressure changes and an increase of falls. A more client-driven care model – with an educated staff and patient – can make a huge difference in outcomes and cost savings, Moffit said.
Evaluating what works and what doesn’t was the core thesis behind Sentara’s care model shift.
Moffit is encouraged by the shift Sentara, his company and others are making to become more conscientious operationally.
“I love that, because now we’re actually going back to evaluate,” he said. “I think in the past, our industry was always go, go, go. Whereas now, we’re trying to find ways to slow down, take the time to self-scout ourselves, so we’re not always chasing our tail. That way, we can get ahead of some of these things and that’s when you start making positive changes.”
The post Home Health Providers Are ‘Self-Scouting’ To Improve Their Own Care Models appeared first on Home Health Care News.