In the first six years of the Home Health Value‐Based Purchasing (HHVBP) Model demonstration, the nine participating states saved Medicare $1.38 billion, a 1.9% decline relative to the 41 non‐HHVBP states.
That’s according to a new study from the U.S. Centers for Medicare & Medicaid Services (CMS) that evaluated the first six years of HHVBP before the national expansion at the beginning of 2023.
The HHVBP Model was implemented to incentivize home health agencies to improve the quality of care they provide to Medicare beneficiaries.
The goal of the model is to link Medicare reimbursement to the quality of care, rather than just the quantity or volume of services.
CMS first adjusted Medicare payments by up to 3% in 2018, using home health agencies’ 2016 Total Performance Score (TPS). Payment adjustments increased each year, peaking at up to 7% in 2021.
With the nine-state trial in the rearview mirror, CMS’ study shows both positives and some negatives, with the HHVBP model.
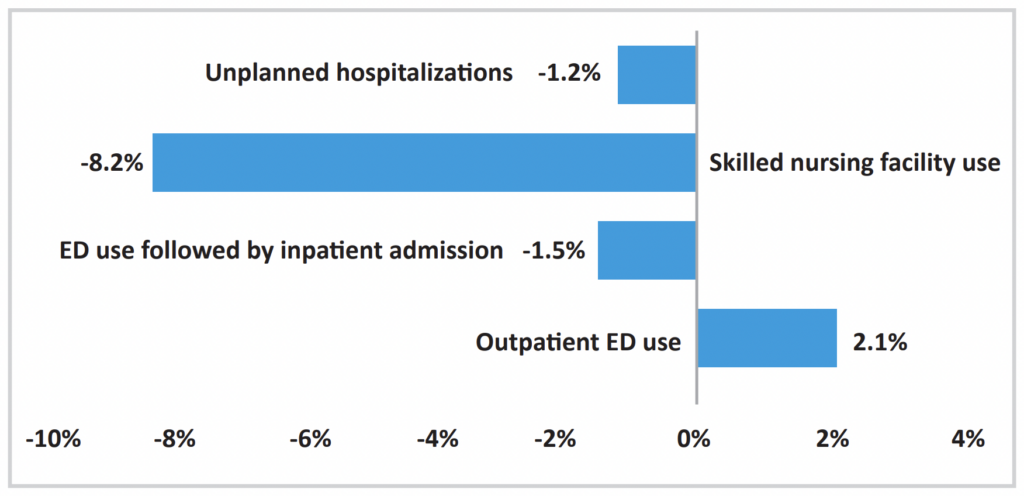
While saving Medicare over $1 billion, providers under the HHVBP pilot also reported reductions in unplanned hospitalizations, skilled nursing facility use and gains in functional status for patients like mobility and self‐care.

The reductions in Medicare spending were largely driven by reductions in skilled nursing facility services ($235.8 million decrease), inpatient hospitalization stay ($807.0 million decrease) and home health spending ($283 million decrease).
Home health agencies in HHVBP states also received higher TPS scores than agencies in non‐HHVBP states for each of the six years.
Agencies reported modest improvement in patients’ mobility, the management of medications and self‐care due to the value-based model. A higher number of patients were discharged into the community rather than institutional care in the HHVBP model.
Room for improvement
While the value-based model showed improvements in nearly every OASIS-based quality measure, agencies did report an increase in outpatient emergency department (ED) visits.

“We examined additional utilization measures and found HHVBP led to cumulative declines in SNF use and ED use followed by inpatient admission, but there was no cumulative impact of HHVBP on overall ED use,” CMS wrote in its study. “Together, these results suggest that the increase in outpatient ED use attributed to HHVBP is related to the reduced likelihood of ED use followed by an inpatient hospital stay.”
The post Home Health Agencies Made The HHVBP Model Demonstration A Resounding Success appeared first on Home Health Care News.